|
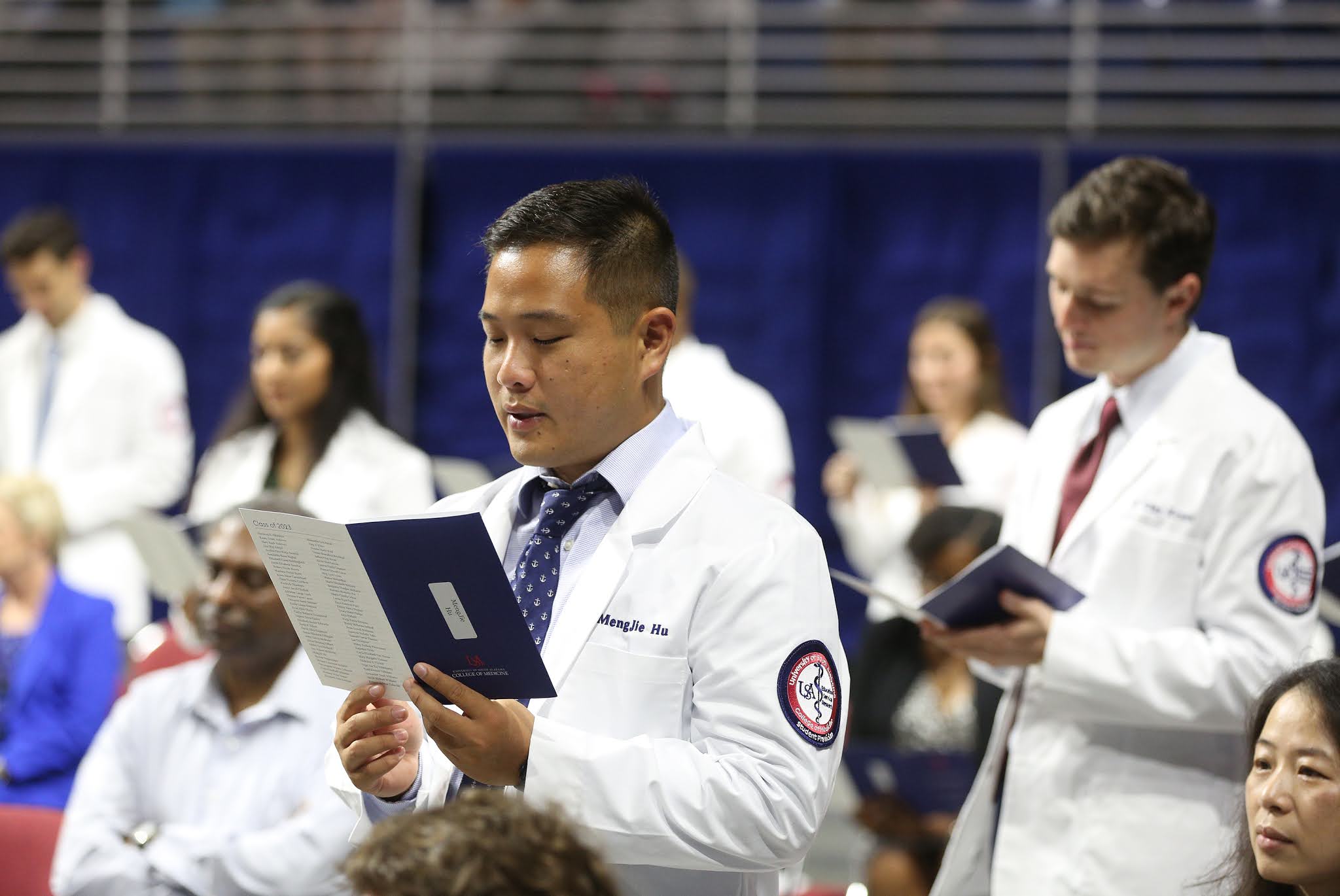
| USA College of Medicine faculty, medical students and resident physicians participated in the American College of Emergency Physicians' Emerald Coast Conference in Destin, Fla. |
Students from the USA College of Medicine won two of the top awards at the American College of Emergency Physicians’ Emerald Coast Conference, held earlier this month in Destin, Fla.
The USA College of Medicine and the Department of Emergency Medicine sponsored a group of medical students and resident physicians in the 10-state regional poster competition.
“This is a first for us, as we have never won so many awards at this annual conference,” said Michael Sternberg, M.D., professor of emergency medicine and medical student clerkship director, who has taken multiple students to the competition in the past 10 years. “We were competing against emergency medicine programs from Oklahoma, UAB, LSU, Kentucky and Vanderbilt; and we excelled.”
 |
Medical students Christopher Evers and Lily Brooks won first place for their poster. |
Fourth-year medical students Lily Brooks and Christopher Evers won first place in the medical student category for their poster presentation titled “My Neck Hurts.” The case dealt with a patient who, while riding a small motorcycle at a backyard party, struck his neck on a clothesline and required emergency intubation and surgical intervention.
“The patient's voice was very hoarse, and air was rapidly expanding under the skin along the neck, a warning sign for serious neck trauma,” Evers said. “We thought this was a great case because the general consensus on how to treat neck trauma has shifted over the years, so we were able to highlight the newer recommendations.”
Evers said the conference was a great opportunity for medical students to practice presenting cases. “One of the responsibilities that comes with being a physician is being an educator,” he said. “We are expected to drive medicine forward and share our discoveries and techniques with others, so that we all can provide the best care possible. The best educators are also compelling and effective communicators. That's why I think this case was successful; it tells a great story.”
Evers acknowledged Sternberg for his guidance on the case: “We couldn’t have done it without him.”
Alicia Hereford and Anna Wright, both fourth-year students, were runners-up in the medical student category for their poster presentation titled “A Rare Cause of Pneumonia.” The case involved a patient with Churg-Strauss syndrome, also known as eosinophilic granulomatosis with polyangiitis, a rare disease that causes inflammation of the blood vessels. This inflammation can restrict blood flow and cause serious, sometimes permanent, damage to organs and nerves.
“Based on the qualities of progression in this disease, early intervention and treatment are critical to prevent irreversible end-organ damage,” Hereford said. “In most cases, Churg-Strauss responds very well to glucocorticoids, with our patient showing great improvement in symptoms within two days.”
Christopher Musselwhite, M.D., a second-year emergency medicine resident and a 2019 USA COM graduate, was runner-up in the resident poster category. His presentation, titled “The Good, the Bad, and the Spleen,” was about a man who was pursued by a bounty hunter. The man was shot by a bean bag round, resulting in a grade 5 splenic laceration that required an emergent splenectomy.
“Presenting a case presentation poster makes you take a deeper dive into a topic, obtaining a better understanding by stepping back and looking at the literature,” Musselwhite said. “Conferences allow you to break out of your local bubble and hear different perspectives on various topics.”
Faculty presenters at the conference included Edward Panacek, M.D., M.P.H., professor and chair of emergency medicine; Larry Mellick, M.D., professor and division chief of pediatric emergency medicine; and Blake Briggs, M.D., assistant professor of emergency medicine.
Sternberg has served as president of the Alabama Chapter of the American College of Emergency Physicians. He was re-elected to the board of the directors at the conference.